Regardless of how seriously a company takes workplace safety, accidents and injuries are bound to happen from time to time. When complex injuries occur, injured employees often need the support of someone to explain medical procedures, help develop customized treatment plans and guide them through recovery. At the same time, companies often need an outside resource to provide quality control over the claims process and ensure the employee is receiving proper medical care.
The challenge is finding someone qualified to act as a helpful resource and steadfast advocate for employees and employers alike. As a solution to this challenge, many companies have turned to nurse case managers. To help explain what nurse case managers do and how they help companies and injured workers manage workers’ compensation claims, we turned to Suzie Burdette, the Vice President of Clinical Operations, Field Case Management at Sedgwick.
Recently, Burdette joined us for our regular Risk Control Webinar Series to talk about nurse case managers in more detail. Here’s a recap of her webinar — The Benefits of Nurse Case Management and the Impact on Claims — which we re-formatted as answers to common questions on the topic.
When it comes to workers’ compensation claims, nurse case managers are charged with overseeing injured employees’ medical care while reducing the total cost of risk for employers. According to Burdette, nurse case management includes several key components like:
As an advocate for injured workers, it’s a nurse case manager’s job to make sure that patients receive treatment plans tailored to each individual’s specific condition and medical history. Providing this level of high-touch care ensures workers get the right treatment for them and that companies don’t have to pay for extraneous medical care. To accomplish this, nurse case managers handle functions like:
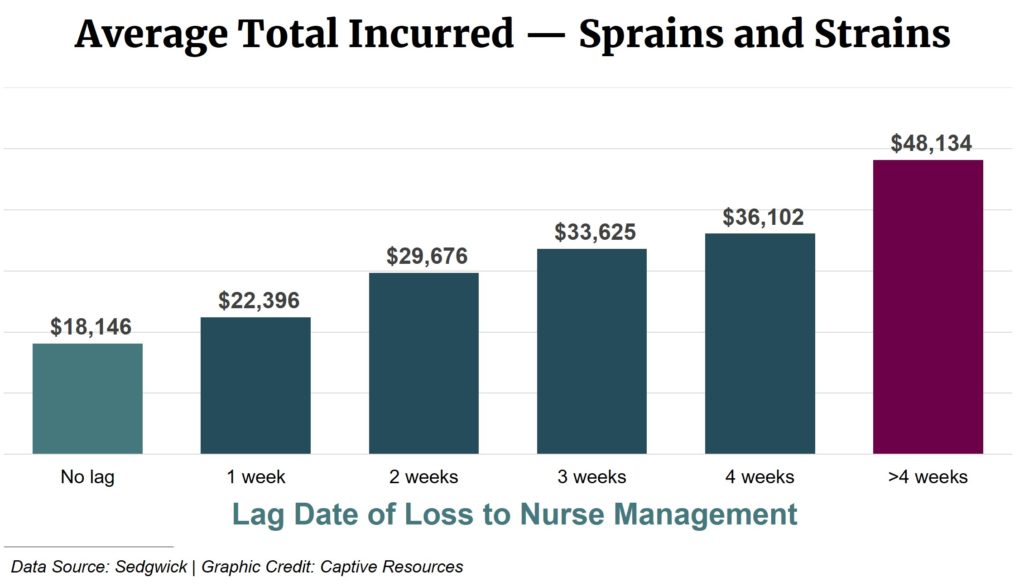
According to Burdette, the best time to bring in a nurse case manager is as soon as possible for many injuries. Based on the numbers from the chart below, instances when companies brought in a case manager right away resulted in 165 percent lower costs than when the company waited a month or more.
“Yes, you might pay a little for the nurse now,” Burdette said. “But if the file gets closed at the earlier point rather than later one, you’ve made that money back.”
Unfortunately, there isn’t a single, simple answer to this question, although there are models to automate the process (more on that in a bit). Still, Burdette did provide signs to help you identify when to bring in a nurse case manager:
“Hands down, a person with catastrophic and complex issues — like someone who’s not healthy to begin with (and) has an injury on top of that — definitely needs a nurse case manager,” said Burdette. In these cases, “there’s a lot of potential problems that can occur. You need someone to help them navigate that.”
According to Burdette, there are three main ways that nurse case managers are brought in to manage a workers’ compensation claim.
Insurance adjusters often recommend bringing in a nurse case manager to help handle more complicated cases. According to Burdette, adjuster advocacy is the traditional method for bringing in nurse case managers.
This method involves a service we covered in another Risk Control Webinar — nurse triage services. In these cases, a triage nurse responding to a workplace injury identifies that the situation warrants bringing in a case manager.
This method has grown in recent years as technology allows us to parse massive data sets to identify common trends. Companies like Sedgwick use predictive analytics to identify claims that could benefit from assigning a nurse case manager based on factors like:
Click here to learn more about Sedgwick’s comprehensive set of business solutions.
This presentation was part of Captive Resources’ Risk Control Webinar Series — weekly installments of webinars to educate the group captive members we work with on topics like workplace safety, organizational leadership, and company performance. The thoughts and opinions expressed in these webinars are those of the presenters and do not necessarily reflect CRI’s positions on any of the above topics.